Introduction:
Needle decompression and thoracostomy are lifesaving emergency procedures performed to alleviate tension pneumothorax, one of the leading causes of preventable death in pre-hospital trauma care and on the battlefield. This guide dives deep into the understanding, performance, and mastery of these interventions, covering everything from the choice of decompression site, the progression from needle decompression to simple thoracostomy, and even the transition to chest tube thoracostomy.
Section 1 – Needle Decompression:
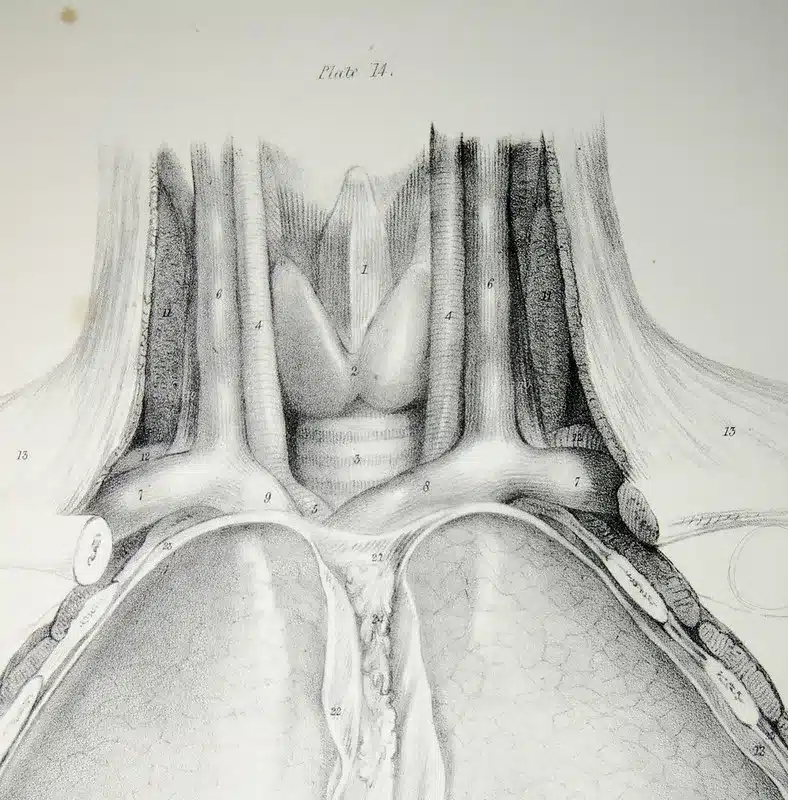
Needle decompression is an immediate intervention performed when a tension pneumothorax is suspected. This critical condition occurs when air accumulates in the pleural space, causing increased pressure that impairs lung function and cardiovascular stability. In this procedure, a needle is inserted into the thoracic cavity to allow trapped air to escape, temporarily relieving pressure and allowing time for definitive treatment.
The preferred site for needle decompression has been the second intercostal space in the mid-clavicular line. However, studies like that of Benns et al. (2015)[^1^] suggest that the fifth intercostal space in the anterior axillary line may have a higher success rate due to the increased chest wall thickness at the traditional site. Despite this controversy, both locations are recognized as appropriate decompression sites, and the choice often depends on the clinician’s training and the patient’s body habitus.
Section 2 – Progression to Simple Thoracostomy:
While needle decompression can be life-saving, it’s not always definitive. In cases of recurrent or ongoing air leaks, or when needle decompression fails to improve symptoms, progression to simple thoracostomy may be warranted. This procedure involves the creation of a small incision at the fifth intercostal space, allowing a finger to be inserted to confirm the presence of free air and relieve tension. Simple thoracostomy offers the advantage of being less likely to become occluded compared to needle decompression, providing a more reliable and durable relief of tension pneumothorax.
Section 3 – Advancement to Chest Tube Thoracostomy:
When more definitive management is needed, or in cases of hemothorax or ongoing air leak, chest tube thoracostomy may be indicated. In this procedure, a chest tube is inserted into the pleural space to remove air, blood, or other fluids, restoring negative pressure and allowing the lung to re-expand. The choice between simple thoracostomy and chest tube thoracostomy often depends on the available resources, the patient’s clinical status, and the provider’s comfort level and training with each procedure.
Section 4 – Battlefield and Pre-Hospital Scenarios:
In battlefield or pre-hospital settings, rapid and effective intervention is crucial. Due to the austere environment, the emphasis is often on quickly recognizing tension pneumothorax and initiating immediate treatment. Needle decompression is typically the first-line intervention due to its speed and simplicity. However, simple thoracostomy is gaining acceptance as a primary intervention in pre-hospital care and on the battlefield, particularly in prolonged field care scenarios where evacuation may be delayed.
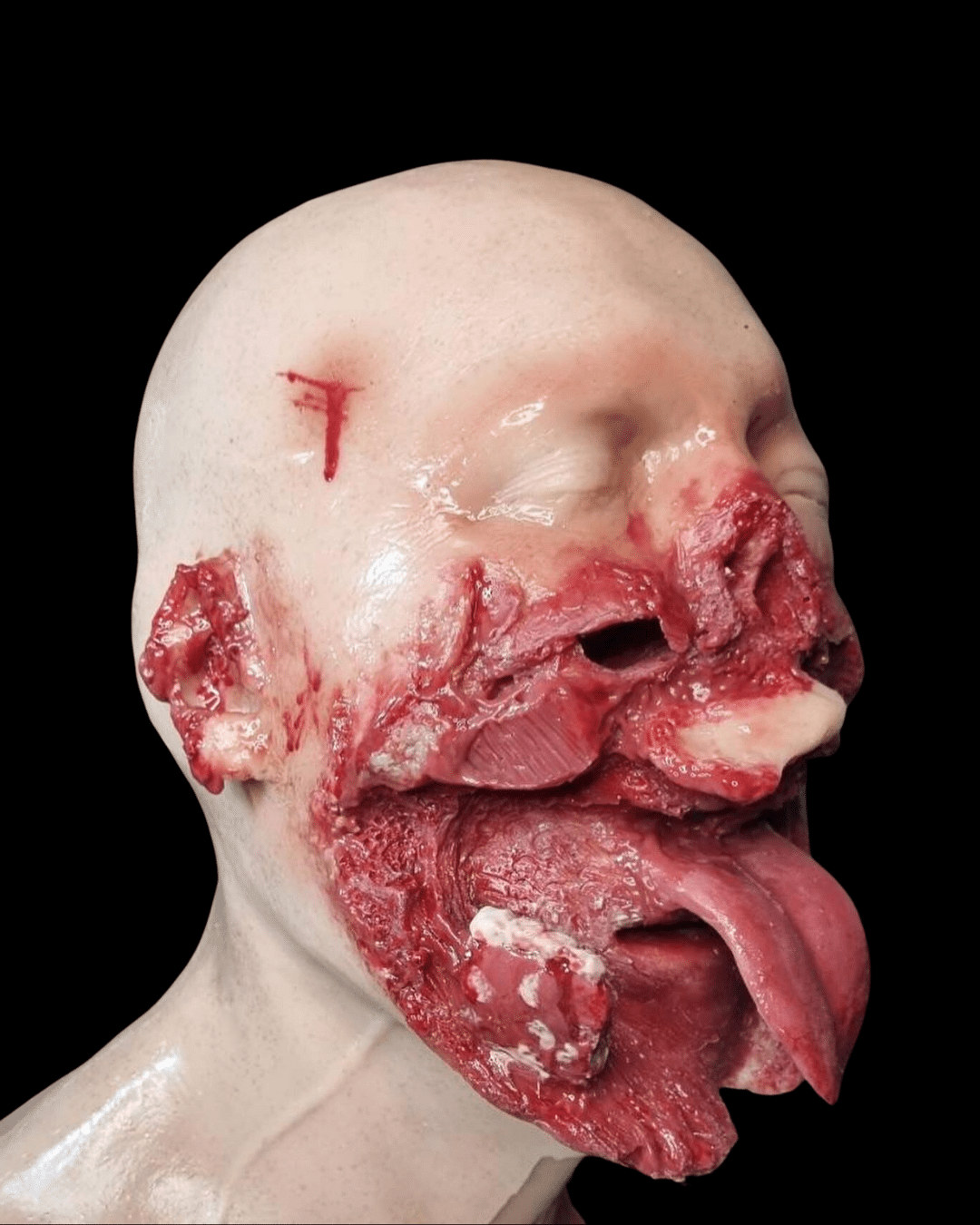
Section 5 – Training Tools: Desktop NCD and Simple Trainer, Wearable Trainer for Simple Thoracostomy:
Proper training is essential to ensure effective and safe performance of these procedures. To facilitate realistic, hands-on practice, Battlefield Partners has developed the Desktop NCD and Simple Trainer, and the Wearable Trainer for SIMPLE’s. These innovative tools offer realistic practice scenarios to help healthcare providers gain proficiency and confidence in these life-saving procedures.
Section 6 – Conclusion:
Mastering needle decompression and thoracostomy procedures is critical to saving lives in emergencies, battlefields, and pre-hospital situations. Continued practice and training using realistic training tools like those offered by Battlefield Partners can help ensure clinicians are well-prepared when they encounter these conditions in the field.
[^1^]: Benns M, Egger M, Day M, et al. Is routine tube thoracostomy necessary after prehospital needle decompression for tension pneumothorax? Am Surg. 2015;81(2):141-146.