Introduction:
In an ever-evolving landscape of emergencies and threats, introducing Tactical Emergency Casualty Care (TECC) marks a turning point in prehospital trauma care. Stemming from its military counterpart, Tactical Combat Casualty Care (TCCC), TECC was developed with the civilian arena in mind, focusing on managing casualties in complex emergencies such as mass shootings or natural disasters. This article delves into TECC’s inception, its comprehensive curriculum, and how Battlefield Partners contributes to improving TECC training with innovative solutions.
Section 1 – The Genesis of TECC:
Born out of necessity, TECC emerged as an equivalent civilian-focused trauma management approach to the military-centric TCCC. Recognizing the need for a system to address injury patterns and specific needs in civilian high-threat situations, the Committee for Tactical Emergency Casualty Care (C-TECC) introduced TECC in 2011[^1^]. Built on battlefield-proven, data-driven guidelines, TECC has been tailored to meet the nuances and complexities of civilian trauma scenarios.
Section 2 – The TECC Curriculum:
The TECC curriculum follows a distinct three-phase model, adapted for the civilian context but bearing a resemblance to TCCC:
- Direct Threat Care (DTC): This phase encompasses care given when under an immediate threat. The primary goal during DTC is to suppress the threat and move the casualty to safety. The focus here is on controlling massive bleeding, the most preventable cause of death in trauma cases.
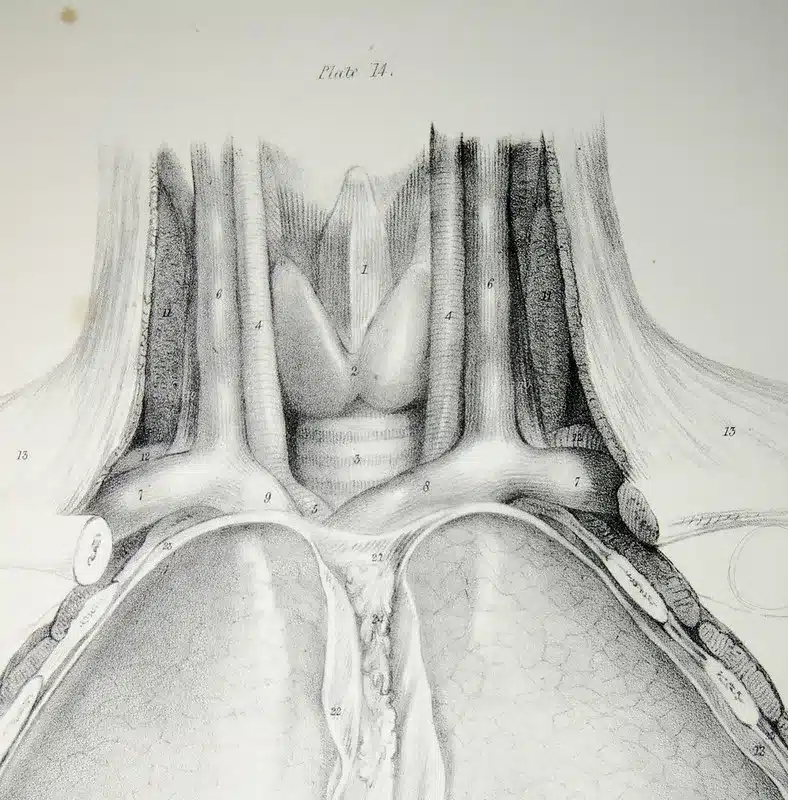
- Indirect Threat Care (ITC): This phase focuses on rapid and effective medical interventions once the immediate threat has been addressed. Here, healthcare providers can perform a more thorough assessment and apply more comprehensive medical care, such as airway management and secondary haemorrhage control.
- Evacuation Care (Evac): In this phase, attention is given to providing care while transporting the casualty to a higher level of medical care. Interventions during this phase might include advanced airway procedures, fluid resuscitation, and treatment for hypothermia.
Section 3 – Essential Skills Acquired Through TECC Training:
TECC equips participants with crucial skills for managing casualties in high-threat civilian environments. These include:
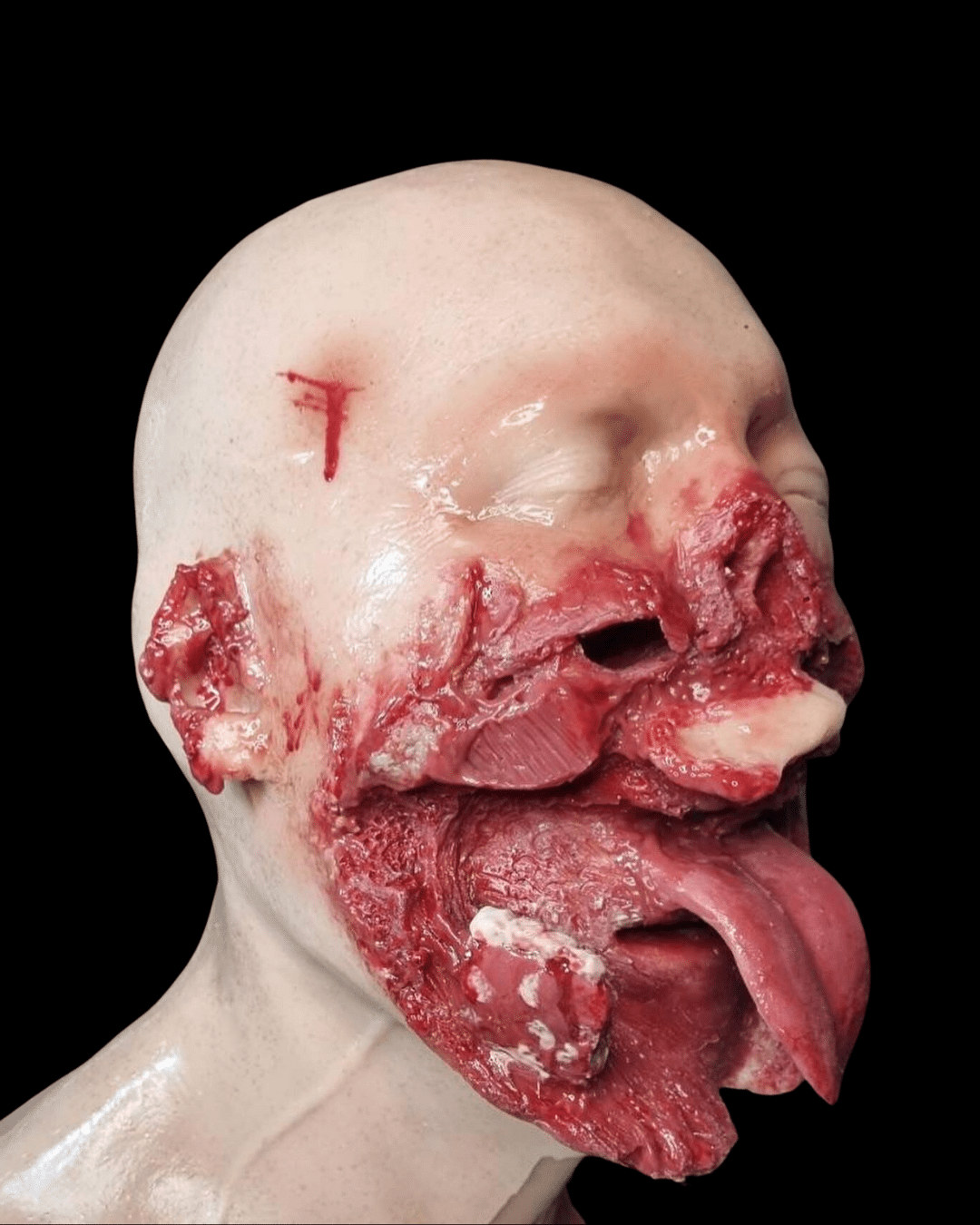
- Haemorrhage control: Using tourniquets, pressure bandages, and wound packing materials to control bleeding[^2^].
- Airway management: Techniques for securing a compromised airway, from basic manoeuvres to more advanced interventions such as surgical cricothyrotomy.
- Respiratory management: Application of chest seals and performance of needle decompression to manage chest injuries.
- Circulation management: Initiating shock management measures and fluid resuscitation to maintain blood flow to vital organs.
- Casualty extrication and evacuation: Learning to effectively and safely move and transport casualties to higher echelons of care.
Section 4 – Battlefield Partners: Enhancing TECC Training:
Battlefield Partners supports TECC training through cutting-edge products that provide a realistic training environment. We offer tourniquet trainers, airway management trainers, chest seal trainers, and wound packing trainers, aiding in practical honing skills and enhancing the ability to save lives in high-threat civilian scenarios.
Section 5 – Conclusion:
TECC offers an innovative approach to civilian prehospital trauma care, effectively managing casualties in high-threat environments. As TECC continues to influence best practices, Battlefield Partners remains committed to supporting this critical training with our specialized products.
Citations:
[^1^]: Callaway, D. W., Smith, E. R., Cain, J., Shapiro, G., Burnett, W. T., McKay, S. D., & Mabry, R. L. (2011). Tactical Emergency Casualty Care (TECC): guidelines for the provision of prehospital trauma care in high threat environments. Journal of Special Operations Medicine, 11(3), 104-122.
[^2^]: Jacobs, L. M., Burns, K. J., & Gross, R. I. (2013). The Hartford Consensus: THREAT, a medical disaster preparedness concept. Journal of the American College of Surgeons, 217(5), 947-953.